Abstract
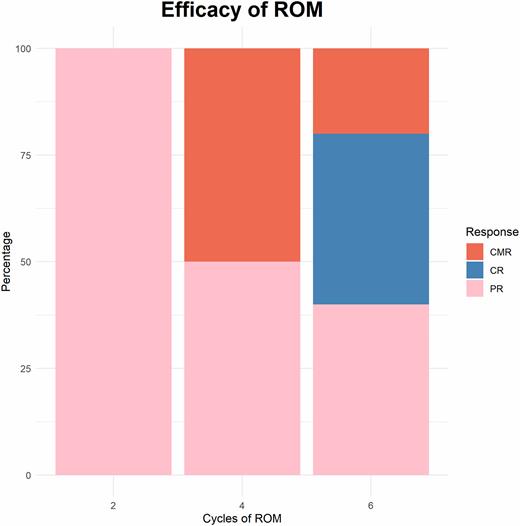
Background: Primary central nervous system lymphoma (PCNSL) is primarily large B-cell lymphoma (accounting for nearly 95% of central lymphomas). Current treatments, including surgery, chemotherapy, and whole-brain radiotherapy, often fail to achieve satisfactory results, especially in the elderly. High-dose methotrexate (MTX) based treatment is the current standard treatment, but the long-term survival rate of young patients is still less than 50% even after autologous transplantation. Bruton's tyrosine kinase (BTK) inhibitor, ibrutinib, has been tested in multiple clinical trials for PCNSL, as a single drug achieved an objective response rate (ORR) of 50-70% and a CRR of 20%-40% in relapsed and refractory PCNSL, while combination therapy can achieve an ORR of 80% and a CRR of 50%. However, ibrutinib efficacy is less than half a year and has poor selectivity. Owing to its off-target inhibition effect, the incidence of serious adverse reactions such as bleeding and atrial fibrillation in patients increases, leading to dose reduction or drug withdrawal, which makes patients unable to continue treatment. Orelabrutinib is a new-generation BTK inhibitor, that has been rationally optimized in molecular structure, which makes its binding with BTK more durable, more stable, more specific, less off-target effect, and higher BBB pass rate and better safety. In addition, a retrospective article published recently showed that obrutinib monotherapy was more effective and well-tolerated in patients with r/r PCNSL. Herein, we combined rituximab, MTX, and ibrutinib for induction therapy, finally through autologous hematopoietic stem cells consolidation therapy or lenalidomide or obrutinib maintenance treatment, to evaluate toxicity and to improve efficacy. This study is registered with Chictr.org.cn, number ChiCTR2200061485. Methods: The study is a multicenter, single-arm, prospective phase II study, conducted at Shengli Oilfield Central Hospital and Shandong Cancer Hospital. Patients diagnosed with Newly Diagnosed PCNSL by biopsy of brain lesion, systemic immunology, bone marrow, and a CSF examination, et al, and be suitable for the immunochemotherapy, were enrolled in the clinical trial. The Orelabrutinib -based ROM regimen consists of rituximab 375mg / m 2 on day 0. MTX 3.5g/m 2 on day1, and Orelabrutinib 150mg once daily on day1 to day 28. Every 28 days is a cycle of treatment. After 4-cycles of ROM induction therapy, patients who achieved CR/CRu/PR received autologous peripheral blood hematopoietic stem cell transplantation (HSCT) or the extra 2 cycles of ROM regimen as consolidation therapy. Orelabrutinib or lenalidomide monotherapy was prescribed as maintenance therapy, according to the willingness of patients until the disease progresses. The primary endpoint was the safety and efficacy of this regimen in newly diagnosed with PCNSL. Results: There were a real of 10 patients enrolled in this clinical trial, between July 2021 and May 2022. All the patients were pathologically DLBCL, including 7 non-GCB subtypes and 3 GCB subtypes. The median follow-up time was 6.5 (1-12) months up to June 30, 2022. After 4 cycles of ROM induction therapy, complete metabolic remission (CMR) was achieved in 5 patients (50%), partial response (PR) in 5 patients (50%), and the overall response rate (ORR) of induction therapy was 100% (Figure 1). Among responders, 3 (33%) received HSCT, 1 (10%) received RT and 5 (50%) received extra 2 cycles of ROM regimen as consolidation therapy. After the consolidation therapy, 90% of patients (9/10) received maintenance therapy, including 5 who received lenalidomide and 4 who received ibrutinib. The median progression-free survival (PFS) and overall survival (OS) were not achieved. The safety of Orelabrutinib -based regimens have also been evaluated. No grade 4 adverse events were observed. Grade 3 hematologic toxicity included lymphopenia in 1 case and neutropenia in 3 cases. Conclusions: Our data preliminaries indicate that ROM is efficacious and well-tolerated as a first-line regimen in newly diagnosed PCNSL and might effectively improve the survival of these patients. These combined therapies offer a potential new therapeutic strategy. More patients and longer follow-ups are necessary to confirm our conclusion.
Figure 1
Disclosures
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2022 by The American Society of Hematology
2022

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal